Vol. 11 – No. 1 – Winter 2015
Robert D. Kerns, Ph.D.
National Program Director for Pain Management Veterans Health Administration
&
Professor of Psychiatry, of Neurology, and of Psychology Yale School of Medicine
Abstract
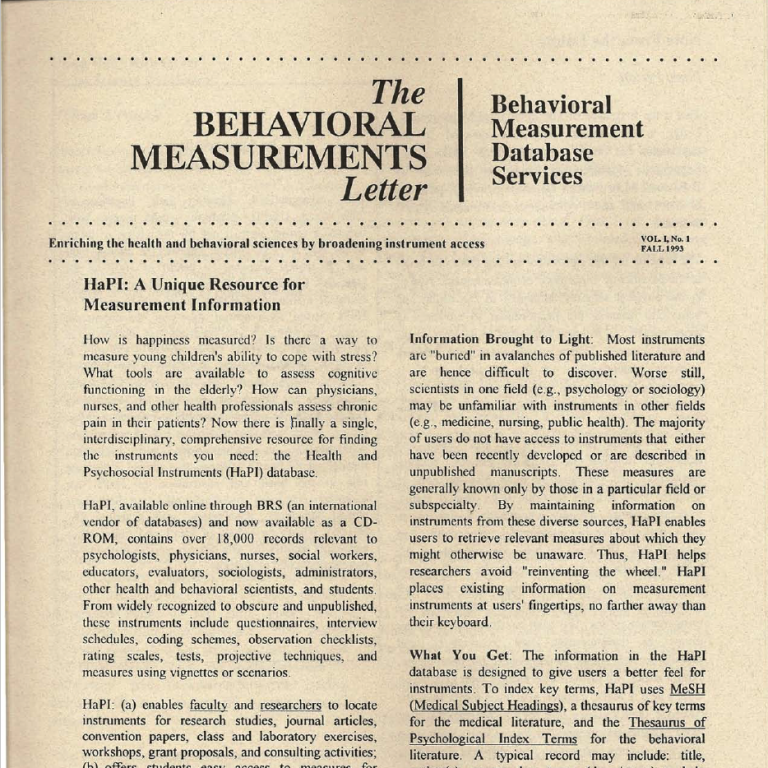
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.1 As a subjective, covert, and personal experience, pain is most commonly assessed using “gold standard” psychometrically sound, standardized self-report measures in the human research and clinical setting. This brief article provides a broad overview of the core domains and most widely employed measures of pain. The Health and Psychosocial Instruments (HaPI) database serves as a key resource for investigators and clinicians alike.
Pain as a Public Health Crisis
The experience of pain is ubiquitous. Pain can be short-lived or acute in the context of an injury, illness, or surgery. Depending on the primary contributor to acute pain and on its severity and expected duration, acute pain may be expected to resolve with little or no intervention. In some circumstances, however, analgesic medications and other therapeutic approaches may be useful to promote reasonable control of pain and optimal physical functioning. Pain that exists longer than usual given the circumstance or longer than ninety days is usually labeled as chronic pain. Chronic pain is commonly associated with a range of musculoskeletal (e.g., osteoarthritis) and neurological (e.g., peripheral neuropathy) disorders. A seminal report from the Institute of Medicine suggested that as many as 100 million Americans, approximately one-third of all adults, report chronic pain at a cost of between $500 and $635 billion per year.1
Although for many persons with chronic pain, pain and its potential negative impacts are well managed, for others, chronic pain may be associated with moderate to severe physical disability, including loss of work and declines in performance of everyday activities. It may also be associated with significant emotional distress and a general decline in quality of life. A large body of research documents that chronic pain is commonly comorbid with mood and anxiety disorders, post-traumatic stress disorder, and substance use disorders.2 Some experts have begun to refer to the concept of “high impact chronic pain” to distinguish chronic pain that significantly affects quality of life from chronic pain that is generally well tolerated. Management of chronic pain, particularly high impact chronic pain, often requires an integrated, patient-centered, multimodal, and interdisciplinary approach to achieve optimal outcomes.3 Unfortunately, pain is also all too often associated with life threatening illnesses, such as cancer, and their treatments. Management of pain at the end of life is a high priority for patients and families, and use of high potency opioid analgesics is commonly required in this setting.
Due to the high prevalence and costs of pain, as well as evidence of disparities in pain care, the Institute of Medicine labeled pain, particularly chronic pain, as a public health crisis, and called for a national transformation in pain prevention, care, research, and professional and public education. In response to this call, a National Pain Strategy is being developed.4 Among its many recommendations, the National Pain Strategy encourages continued efforts to develop reliable tools for the measurement of pain for use in multiple settings, including basic laboratory, epidemiological, and translational, pre-clinical, clinical, and health services research settings, as well as in the context of health services delivery in clinical and rehabilitation settings. In the pre-clinical and clinical research setting, for example, investigators are employing functional neuroimaging to develop knowledge about the central representation of pain, including innovative applications for studies of such phenomenon as emotional and social aspects of pain.5 The Behavioral Measurement Letter Vol. 11, No. 1, Winter 2015 In the past several years, novel theories and related constructs have emerged such as pain catastrophizing 6 and fear avoidance 7 and reliable measures of these constructs have emerged that help to explain the maintenance, if not the development, of chronic pain for some individuals. In the clinical practice setting, investigators continue to search for novel, pragmatic approaches that can be used to inform an understanding of persons’ idiosyncratic experiences of pain and its impact on functioning and well-being. It is within this context that the Health and Psychosocial Instruments HaPI database and its multiple pain-relevant measures are so important, and it is the focus of this brief review.
The Biopsychosocial Model
The biopsychosocial model has emerged as the predominant framework for conceptualizing pain, chronic pain, and pain management.8 First introduced by George Engel in 1978, the biopsychosocial model emphasizes the inter-relatedness of biological, psychological, and social factors in the context of disease and health. Consistent with this model, the experience of pain is conceptualized as a function of such nociception associated with structural pathology as well as a range of psychosocial factors, including mood, attention, appraisal, and social context. This model largely explains the wide variation in pain intensity, functional status, and emotional distress observed among people with similar injuries. The model also helps to illuminate the multiple dimensions of the chronic pain experience and targets for intervention, including the underlying painful medical condition and pain itself, as well as functional limitations and emotional distress.
Informed by the biopsychosocial model, the National Pain Strategy specifically calls upon clinicians “to undertake comprehensive assessments of patients with chronic pain, leading to an integrated plan of coordinated care, managed by an interdisciplinary team, when necessary.”4 In addition to a thorough history and physical examination, psychological and behavioral assessment of pain is also strongly indicated in many, if not most, clinical settings. A multidimensional psychological and behavioral assessment serves as a foundation for treatment planning and subsequent evaluation of treatment outcomes. Psychological and behavioral assessment may also reveal the need for adjunctive psychological treatment of preexisting or emerging psychosocial difficulties that may interfere with medical treatments of painful conditions. Psychological assessment can provide information about patients’ motivation and readiness to engage in treatment and their treatment preferences. Finally, psychological assessment can provide data about a patient’s suitability for surgical or other invasive procedures under consideration.
Core Domains of Comprehensive Pain Assessment
A broad array of approaches and standardized measures are commonly employed. Of course, a core foundational principle of pain assessment is the fact that pain is essentially a private, covert, and subjective experience. As such, many would argue that “pain is what the person says it is,” and others’ respect for persons’ reports of pain is essential as a basis upon which to explore the biopsychosocial context of that experience. Self-report of pain and its impacts can be obtained by any of several assessment strategies such as interviews, standardized questionnaires, and diaries. These common assessment approaches can be complemented by behavioral observation, psychophysiological assessment, and assessment of family members and significant others. The use of multiple, standardized assessment measures is encouraged to obtain comprehensive, valid, and reliable information.
It is in this context that the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) has identified core domains for pain assessment and has recommended specific measures for capturing each domain.9,10 Details regarding IMMPACT and the numerous publications that have emerged from this initiative are available at www. immpact.org. IMMPACT recommends explicit attention to six primary domains when assessing pain, especially chronic pain, and particularly in the context of clinical efficacy and effectiveness trials: (1) pain, (2) physical functioning, (3) emotional functioning, (4) patient ratings of improvement and satisfaction with treatment, (5) symptoms and adverse events, and (6) patient disposition. Among criteria for evaluating and selecting specific measures, IMMPACT recommended that the following parameters be considered: (1) appropriateness of the measure’s content and conceptual model, (2) reliability, (3) validity, (4) responsiveness to change, (5) interpretability, (6) precision of scores, (7) respondent and administrator acceptability, (8) respondent and administrator burden and feasibility, (9) availability and equivalence of alternate forms and methods of administration (e.g., self-report versus interviewer), and (10) availability The Behavioral Measurement Letter Vol. 11, No. 1, Winter 2015 and equivalence for different cultures and languages.
Measures of Pain Intensity and Quality
As already emphasized, self-report is the gold standard for assessing pain severity or intensity, and quality. Three specific pain severity measures have garnered the largest proportion of attention in the literature, and each has substantial evidence supporting its psychometric properties including reliability, validity, and responsivity to change. The numeric rating scale (NRS) is the most commonly employed measure of pain severity. Typically respondents are asked to rate their level of pain on a zero (no pain) to 10 (worst pain imaginable) scale. The instructions may vary in terms of specific parameters for the report. For example, although it is most common to inquire about pain “now,” respondents may also be asked to report on average, least and worst pain over a specified period, for example, over the past day or week. The visual analogue scale (VAS) typically involves a 100 cm scale with similar anchors to the NRS, and respondents are asked to make a mark on the line that best represents their pain intensity level. The verbal rating scale (VRS) typically uses a small list of adjectives that are intended to quantify the experience of pain severity, namely none, mild, moderate, and severe. After careful consideration of the data on each of these options, IMMPACT recommended use of the NRS in most situations.10 Consistent with this recommendation, many healthcare organizations have adopted the NRS for routine screening for the presence and intensity of pain in clinical settings, often referring to “Pain as the fifth vital sign.”11 IMMPACT also noted that alternative approaches to assessing pain severity may be adopted when such measures exist for specific clinical conditions. For instance, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) is sometimes used to assess pain associated with osteoarthritis.12
Perhaps the most commonly used self-report measure of pain is the McGill Pain Questionnaire (MPQ), a more lengthy measure designed to assess the quality and affective component of the pain experience, not simply pain intensity.13 Respondents choose pain descriptors from a list of 78 potential descriptors that fall into 20 pain categories. These descriptors assess four pain domains: sensory, affective, evaluative, and miscellaneous. Within each category, the individual descriptors reflect varying degrees of intensity and are assigned corresponding numerical values that reflect this difference. Respondents also highlight the location of their pain on a figure drawing and provide information about the factors that alleviate and aggravate their pain intensity. The MPQ generates three scores: (1) the Pain Rating Index, which is the sum of all words chosen in the available categories (the sum of the value of each subclass can be obtained also); (2) Number of Words Chosen, a score that reflects the number of words chosen from each of the four categories; and (3) the Present Pain Intensity, a rating of current pain on a scale from 0 (no pain) to 5 (excruciating). The MPQ has been widely used in a variety of pain-focused research and has been translated into several languages, though not all new versions of the scale have been subjected to adequate clinometric or psychometric testing. A 15-item short-version of the MPQ (SF-MPQ) is also available.14 The IMMPACT committee recommends the use of the SF-MPQ as a measure of pain quality and the affective component of pain, as these aspects of the pain experience may respond differently to treatment than pain intensity.
Psychosocial Context of Pain
Also consistent with the biopsychosocial model of pain, assessment of the psychosocial and emotional context and impact of pain has also been strongly recommended. Among the first and most widely used measure of psychosocial dimensions of the experience of chronic pain is the West Haven–Yale Multidimensional Pain Inventory (WHYMPI)15—a 52-item multi-faceted self-report instrument that employs 7-point Likert scales. The WHYMPI consists of three sections. Section one includes six scales measuring pain-related interference across several domains, including work and leisure activities as well as interpersonal relationships; perceived support from spouse or significant other; pain severity and suffering; perceived life control; and negative mood. Section 2 assesses patient perception of significant others’ responses to overt expressions of pain, classifying responses as solicitous, distracting, or negative. Section 3 measures the frequency with which the patient engages in four clusters of everyday activities including household chores, social activities, outdoor work, and activities away from home. Turk and colleagues have proposed an empirically derived taxonomy of the WHYMPI that includes three reliable profiles of patients with persistent pain labeled as Dysfunctional, Interpersonally Distressed, and Adaptive Copers, and these investigators and several other groups have replicated these findings in numerous samples of The Behavioral Measurement Letter Vol. 11, No. 1, Winter 2015 patients with various pain conditions.15 The measure has been used in numerous empirical studies, including clinical trials of psychological and pharmacological interventions, studies of the psychosocial impact of pain, and studies examining the role of psychosocial factors as contributors to the development and maintenance of persistent pain. The IMMPACT Group recommended the use of the Interference Scale of the WHYMPI for use as an outcome measure in pain clinical trials.6
Numerous additional standardized approaches for the assessment of key dimensions of the chronic pain experience have also been developed and are commonly employed in clinical and research settings. As just one example, the Brief Pain Inventory (BPI) was originally developed to measure pain intensity and interference in patients with cancer pain, but it has been widely used to assess non-cancer pain.17,18 A short-form of the BPI containing 15 items is also available. Demonstrations of its reliability and validity and its availability in multiple languages have contributed to it being recommended by IMMPACT for use as a measure of physical functioning in pain clinical trials.6 The PEG-3 is an ultra-brief version of the BPI consisting of three items: (P) Pain Intensity, (E) Enjoyment of Life, and (G) General Activity. Development studies demonstrated reliability and validity for the PEG-3 comparable to that of the longer BPI.19 The Roland Morris Disability Questionnaire, consisting of 24 items, has been developed specifically for use with patients with chronic low back pain and is also recommended by IMMPACT as a measure of physical functioning.20
Quite recently the National Institutes of Health (NIH) Patient-Reported Outcomes Measurement Information System (PROMIS) has been developed and is being promoted as an enhancement over existing measures. PROMIS is a standardized item bank developed by a cooperative group for the purpose of developing psychometrically sound standardized measures to assess patient-reported outcomes. These measures provide information in the domains of physical, mental, and social health, across a variety of medical illnesses. Measures for pain currently available in the PROMIS assessment center (www.assessmentcenter.net) include Pain–Interference and Pain–Behaviors.21,22 Both measures demonstrated reliability and validity in psychometric evaluation, were related to other measures of pain-related outcomes, and discriminated among groups of patients with differing self-reported health, numbers of chronic conditions, and numbers of disabling conditions. Available studies suggest that these scales provide comprehensive, sophisticated, and psychometrically sound measures for pain-related patient-reported outcomes.
Assessment of the impact of pain on emotional functioning as well as on mental health is also a particularly important consideration, particularly when assessing persons with chronic pain. The rationale for this recommendation includes the high prevalence of emotional distress and comorbid mental health conditions among persons with chronic pain conditions, the negative effects of emotional distress on pain and pain-related disability, the inflated health care costs associated with emotional distress and mental health comorbidities among patients with chronic pain, and the influence of emotional distress and mental health problems on pain treatment participation and outcomes. Key dimensions of emotional distress include depressed mood, anxiety, and anger, and symptoms of mood and anxiety disorders, post-traumatic stress disorder, and alcohol and substance use disorders. For the most part, measurement of these factors involves the use of any of several relevant standardized measures such as the Beck Depression Inventory,23 although there are also a growing number of pain-specific measures that can be considered such as the Pain Anxiety Symptom Scale.24
Beyond these core domains, theory and a burgeoning empirical literature have contributed to the emergence of multiple important constructs and measures of these constructs that are increasingly employed in clinical settings. One of the most important of these emerging constructs is pain coping, which has led to the development of such measures as the Survey of Pain Attitudes,25 the Chronic Pain Coping Inventory,26 and the Pain Catastrophizing Scale.27 Informed by Prochaska’s Transtheoretical Model of Behavior Change, the Pain Stages of Change Questionnaire has been developed as a measure of persons’ readiness to engage in a self-management approach to chronic pain.28
Challenges and Opportunities
Despite the maturity of the field of pain measurement, numerous challenges remain. There is considerable interest and perceived need to develop ultra-brief measures of key constructs for use in epidemiological research and busy clinical practice settings, especially primary care. Development of novel, reliable, and feasible measures of physical function- The Behavioral Measurement Letter Vol. 11, No. 1, Winter 2015 is encouraged, including the use of portable algometry for measuring the minimal amount of pressure that produces pain during activity. Innovative use of technologies such as mobile applications for smartphones and other phone and Internet based approaches also represent exciting new opportunities.29
In closing, it is widely appreciated that the foundation of good pain management is the availability of a comprehensive assessment that is theoretically informed, valid, reliable, and patient-centered. The Health and Psychosocial Instruments (HaPI) database is a state of-the-science resource for the investigator and clinician in search of optimal tools for research and clinical practice. Dr. Evelyn Perloff, the originator of the HaPI database, and her colleagues are to be commended for their extraordinary efforts to develop this invaluable resource and to promote its availability in the service of improving the care of persons with pain.
References
- Institute of Medicine Committee on Advancing Pain Research, Care, and Education (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press.
- Higgins, D. M., Kerns, R. D., Brandt, C. A., Haskell, S. G., Bathulapalli, H., Gilliam, W., & Goulet, J. L. (2014). Persistent pain and mental health disorder comorbidity among Operation Iraqi Freedom and Operation Enduring Freedom veterans. Pain Medicine, 15, 782-790.
- Dorflinger, L. M., Ruser, C., Sellinger, J., Edens, E. L., Kerns, R. D., & Becker, W. C. (2015). Integrating interdisciplinary pain management into the primary care setting: An early phase implementation study. Pain Medicine, 15, 2046-2054.
- National Institutes for Health Interagency Pain Research Coordinating Committee (2015). National Pain Strategy: A comprehensive population health-level strategy for pain. Washington, DC: Department of Health and Human Services (draft).
- Wager, T. D., Atlas, L. Y., Lindquist, M. A., Roy, M., Woo, C.-W., & Kross, E. (2013). An FMRI-based neurological signature of physical pain. New England Journal of Medicine, 368, 1388- 1397.
- Spinhoven, P., Ter Kuile, M., Kole-Snijders, A. M., Hutten Mansfeld, M., Den Ouden, D. J., & Vlaeyen, J. W. (2004). Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. European Journal of Pain, 8, 211-219.
- Rainville, J., Smeets, R. J., Bendix, T., Tveito, T. H., Poiraudeau, S., & Indahl, A. J. (2011). Fear-avoidance beliefs and pain avoidance in low back pain–translating research into clinical practice. Spine, 11, 895-903.
- Gatchel, R. J. (2004). Comorbidity of chronic pain and mental health disorders: The biopsychosocial perspective. American Psychologist, 59, 795-805.
- Turk, D. C., Dworkin, R. H., Allen, R. R., Bellamy, N., Brandenburg, N., Carr, D. B., et al. (2003). Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain, 106, 337-345.
- Dworkin, R. H., Turk, D. C., Farrar, J. T., Haythornthwaite, J. A., Jensen, M. P., Katz, N. P., et al. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113, 9-19.
- Kerns, R. D., Wasse, L., Ryan, B., et al. (2000). Pain as the 5th Vital Sign,Toolkit V.2. Washington, DC: Veterans Health Administration.
- Bellamy N., Buchanan W. W., Goldsmith, C. H., Campbell, J., & Stitt, L. W. (1988). Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. Journal of Rheumatology, 15, 1833-1840.
- Melzack, R. (1975). The McGill Pain Questionnaire: Major properties and scoring methods. Pain, 1, 277-299.
- Melzack, R. (1987). The Short-Form McGill Pain Questionnaire. Pain, 30, 191-197. The Behavioral Measurement Letter Vol. 11, No. 1, Winter 2015
- Kerns, R. D., Turk, D. C., & Rudy, T. E. (1985). The West Haven-Yale Multidimensional Pain Inventory. Pain, 23, 345-356.
- Turk, D. C., & Rudy, T. E. (1988). Toward an empirically derived taxonomy of chronic pain patients: Integration of psychological assessment data. Journal of Consulting and Clinical Psychology, 56, 233-238.
- Cleeland, C. S., & Ryan, K. M. (1994). Pain assessment: Global use of the Brief Pain Inventory. Annals of Academic Medicine, 23, 129-138.
- Keller, S., Bann, C. M., Dodd, S. L., Schein, J., Mendoza, T. R., & Cleveland, C. S. (2004). Validity of the Brief Pain Inventory for use in documenting the outcomes of patients with noncancer pain. Clinical Journal of Pain, 20, 309-318.
- Krebs, E. E., Lorenz, K. A., Bair, M. J., Damuch, T. M., Wu, J., Sutherland, J. M., Asch, S. M., & Kroenke, K. (2009). Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. Journal of General Internal Medicine, 24, 733-738.
- Roland, M., & Morris, R. (1983). A study of the natural history of back pain: Part I. Development of a reliable and sensitive measure of disability in low-back pain. Spine, 8, 141-144.
- Amtmann, D., Cook, K. F., Jensen, M. P., Chen, W. H., Choi, S., Revicki, D., Cella, D., Rothrock, N., Keefe, F., Callahan, L., & Lai, J. S. (2010). Development of a PROMIS item bank to measure pain interference. Pain, 150, 173-182.
- Revicki, D. A., Chen, W. H., Harnam, N., Cook, K. F., Amtmann, D., Callahan, L. F., Jensen, M. P., & Keefe, F. J. (2009). Development and psychometric analysis of the PROMIS pain behavior item bank. Pain, 146, 158-169.
- Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561-571.
- McCracken, L. M., Zayfert, C., & Gross, R. T. (1992). The Pain Anxiety Symptoms Scale: Development and validation of a scale to measure fear of pain. Pain, 50, 67-73.
- Jensen, M. P., Karoly, P. & Huger, R. (1987). The development and preliminary validation of an instrument to assess patients’ attitudes toward pain. Journal of Psychosomatic Research, 31, 393-400.
- Jensen, M. P., Turner, J. A., Romano, J. M., & Strom, S. E. (1995). The Chronic Pain Coping Inventory: Development and preliminary validation. Pain, 60, 203-216.
- Sullivan, M. J. L., Bishop, S. C., & Pivik, J. (1995). The Pain Catastrophizing Scale: Development and validation. Psychological Assessment, 7, 524-532.
- Kerns, R. D., Rosenberg, R., Jamison, R. N., Caudill, M. A., & Haythorn Thwaite, J. (1997). Readiness to adopt a self-management approach to chronic pain: The Pain Stages of Change Questionnaire (PSOCQ). Pain, 72, 227-234.
- Heapy, A. A., Sellinger, J., Higgins, D., Chatkoff, D., Bennett, T. C., & Kerns, R. D. (2007). Using interactive voice response to measure pain and quality of life. Pain Medicine, 8(s3), S145-S154.
Dr. Robert D. Kerns is the National Program Director for Pain Management for the Veterans Health Administration, and Professor of Psychiatry, of Neurology, and of Psychology in the Yale School of Medicine. He has published over 200 peer-reviewed articles, chapters, and books, and frequently delivers invited addresses at professional and scientific meetings. His research has been funded through the VA and through other federal and private sources for over 30 years. His current research focuses on pain and pain care among veterans, mechanisms and processes of change during psychological interventions for chronic pain, the use of innovative technologies to promote access and fidelity of non-pharmacological pain interventions, and formative evaluation and implementation of organizational improvement initiatives in pain care.
winter2015-30th-Anniversary